2013/02/06
Solute carrier family 2 member 1 is involved in the development of nonalcoholic fatty liver disease
Non-alcoholic fatty liver disease (NAFLD) covers a wide spectrum of liver pathologies including steatosis and non-alcoholic steatohepatitis (NASH), and may progress to cirrhosis and its complications such as hepatocarcinoma. NAFLD is the most common cause of chronic liver disease in several western countries with a prevalence of 24% in general population, and about 75% in obese patients, being mostly related with visceral adiposity, obesity, type 2 diabetes mellitus and metabolic syndrome.
Up to now, the only way to diagnose NAFLD with certainty is liver biopsy. The objective of the present project is to discover genetic markers with the aim of further understanding NAFLD occurrence and of proposing potential non-invasive diagnostic methods for this disorder.
STRATEGY
- A total of ninety-two genes were selected to be tested for association to NAFLD.
- The selection of genes was based on transcriptomics, proteomics, and metabolomics studies on the disease, as well as on their relation to one-carbon metabolism, comprising the methylation and folate cycles.
- 3072 SNPs belonging to these genes where genotyped in cases and controls and tested for statistically significant association.
- Associations detected in the first phase were genotyped again for validation in a lager independent cohort of cases and controls.
- The regulation of the genes potentially associated to the disease after validation was tested in liver biopsies using Real-Time PCR.
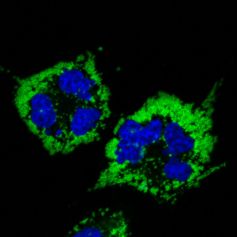
- Derived hypotheses were tested by silencing likely associated genes in THLE-2 cells (human hepatocytes that express phenotypic characteristics of normal adult liver epithelial cells).
In this study we showed that several SNPs of SLC2A1 (solute carrier family 2 (facilitated glucose transporter) member 1) showed association with NAFLD but not with Type 2 Diabetes, being the haplotype containing the minor allele of SLC2A1-sequence related to the susceptibility to develop NAFLD. In addition, gene expression analysis demonstrated a significant down-regulation of SLC2A1 in NAFLD-livers (p-value= 2.7382 x 10-6).
Enrichment functional analyses of the transcriptome profiles drove us to demonstrate that in-vitro silencing of SLC2A1 induces an increased oxidative stress activity and a higher lipid accumulation under oleic acid treatment.
CONCLUSIONS
According to the fact that SLC2A1 protein, GLUT1, is inserted in the plasma membrane of only the last two perivenular hepatocytes in the liver cell plate, exactly in the same cells where steatosis starts in adult NAFLD, we propose that impairment in lipid metabolism in siSLC2A1-cells promotes accumulation of triglycerides. The observed diminished amount of SLC2A1 in the liver of NAFLD patients and the effect of oleic acid medium enrichment in siSLC2A1-THLE2-cells indicate either that the decrease of SLC2A1-mRNA levels induce triglyceride accumulation or vice versa, that a fat rich environment activates some mechanism (e.g.: glucose-fatty acid cycle) that down-regulates the expression of SLC2A1 in hepatic cells. In conclusion, these observations indicate that hepatic SLC2A1 mediates lipid metabolism providing new potential insights into NAFLD pathogenesis.
See a large version of the first picture